What are these new regulations?
The No Surprises Act and Transparency In Coverage Final Rule introduced the most comprehensive reforms to health plans since the Affordable Care Act. Designed to protect consumers against surprise medical bills and provide cost transparency, these regulations impose new requirements that health plan sponsors will have to meet in the coming months and years.
As a plan sponsor, you are responsible for complying with these new requirements. However, as a client of HealthEZ, you’re covered and up to date. We’ve already met current requirements and are on track for future obligations.
EZChoice
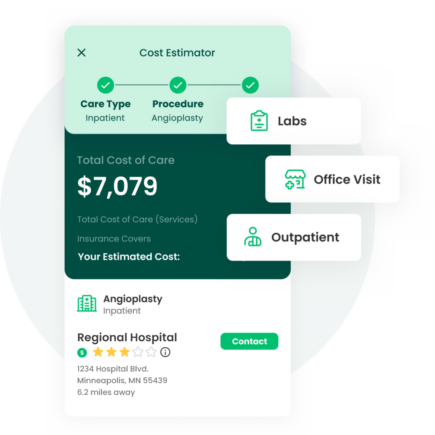
EZchoice, our new cost estimator tool makes provider choice easy and costs transparent.
- Members can shop 500 common services for quality and cost.
- Integrated within our member app for the best experience.
With EZchoice, you can be confident that your plan is compliant, costs are transparent and members are not overspending on care.
I.D. Cards
Get more information right from your new I.D. Card. In 2022, members received updated cards that show their applicable deductible and out-of-pocket limits, plus a telephone number and website for direct customer assistance.
No Surprises Act:
What we are doing to comply
| Requirement | Complete? | Deadline | How we're helping you comply |
|---|---|---|---|
| I.D. Cards | January 2022 | Ensured members received updated I.D. Cards upon renewal in 2022 that included: (1) applicable deductible; (2) out- of-pocket maximum limitations; (3) a telephone number and web address where people can seek customer assistance. | |
| Balance Billing Protections | January 2022 | Gave plan sponsors a compliance notice to post in their workspace, added specific EOB message codes and additional disclosures on NSA eligible claims, and established a process to ensure the allowed amounts are calculated correctly. | |
| Independent Dispute Resolution | January 2022 | Developed a process and notice provision on EOBs sent to providers with the required language on how to dispute NSA-allowed amounts. | |
| Provider Directory | January 2022 | Created a provider directory to ensure that Aetna PPO, Cigna PPO and America’s PPO, our proprietary network, comply with these requirements. | |
| Provider Anti Discrimination Protections | January 2022 | Established a process to ensure network partners comply with these requirements so that plans do not discriminate against any provider acting within the scope of that provider’s license or certification. | |
| Continuity of Care | January 2022 | Confirmed that Aetna PPO, Cigna PPO, and America’s PPO are in compliance with these new protections for continuing care patients against surprise charges when a provider or facility ceases to be in-network. | |
| Reporting on Pharmacy and Drug Costs | December 2022 | The NSA creates new requirements to submit detailed information related to prescription drug spending to the Departments of Health and Human Services, Labor, and Treasury. This information will be used by the Departments to generate a bi-annual report on prescription drug pricing trends and the role of prescription drug costs in the overall cost of a health plan. HealthEZ has established a process to help its clients comply with this new reporting requirement. | |
| Advanced EOBs | TBD | While this requirement is currently delayed, we are proactively preparing so that plan sponsors can create and send an Advanced Explanation of Benefits that includes a “good faith estimate” of the participant’s cost-sharing liability for certain advanced scheduled services. |
Transparency In Coverage:
What we are doing to comply
| Requirement | Complete? | Deadline | How we're helping you comply |
|---|---|---|---|
| Machine Readable File (Out-of-Network Allowed Amounts) | July 2022 | Coordinated on behalf of our self-funded clients to receive and post applicable out-of- network allowed rates on a publicly available website in the Machine Readable File format. | |
| Machine Readable File (In- Network Negotiated Rates) | July 2022 | Coordinated on behalf of our self-funded clients to receive and post applicable in-network negotiated rates on a publicly available website in the Machine Readable File format. | |
| Machine Readable File (Prescription Drugs) | TBD | While this requirement is currently delayed, HealthEZ is proactively preparing a machine-readable file containing negotiated rates and historical net prices for covered prescription drugs. | |
| Price Comparison Tool (500 Items) | January 2023 | Currently developing a new cost estimator tool that will allow plan participants to shop for 500 common services and compare both cost and quality data. This service will leverage claims data, Machine Readable Files and quality data. It will go beyond what is required to satisfy the requirements of the new law. | |
| Price Comparison Tool (All Items) | January 2024 | Currently developing a cost estimator tool for all services prior to the deadline set by TIC. | |
| Price Comparison Tool (Pharmacy) | January 2024 | Currently developing a cost estimator tool for pharmacy services prior to the deadline set by TIC. |
Looking for more detail?
Download the requirements summary to learn more about
each required step, key dates, and associated details.
Have questions about these new requirements? Send us a message or or call us directly

