COST CONTAINMENT
Health plan costs keep rising and fully insured policies don’t bend the curve. We believe that business plans and benefit plans should work in harmony. To that end, we give self-funded plans the freedom to offer affordable, high-quality benefits to their employees.
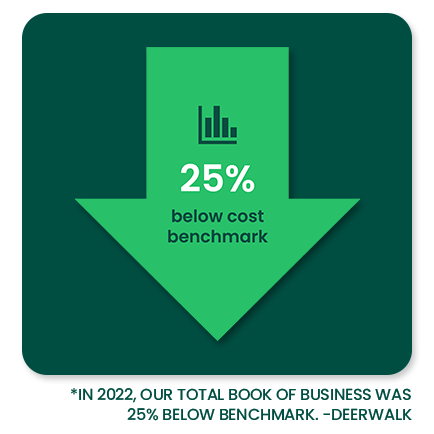
Your bottom line is our incentive.

That’s why we’re here.
No stone
unturned
HealthEZ has a defined road map that’s focused on reducing plan cost while keeping member satisfaction and quality of care high.
Our integrated approach to cost containment is engaged with every step in the continuum of care. To increase engagement and effectiveness, our Care Advocacy team is fully connected with the member.
Our proven approach
to cost containment
We’ve built a comprehensive methodology that engages our cost containment products, solutions and advocacy team at every stage of care. We support members and the plan throughout the continuum of care.
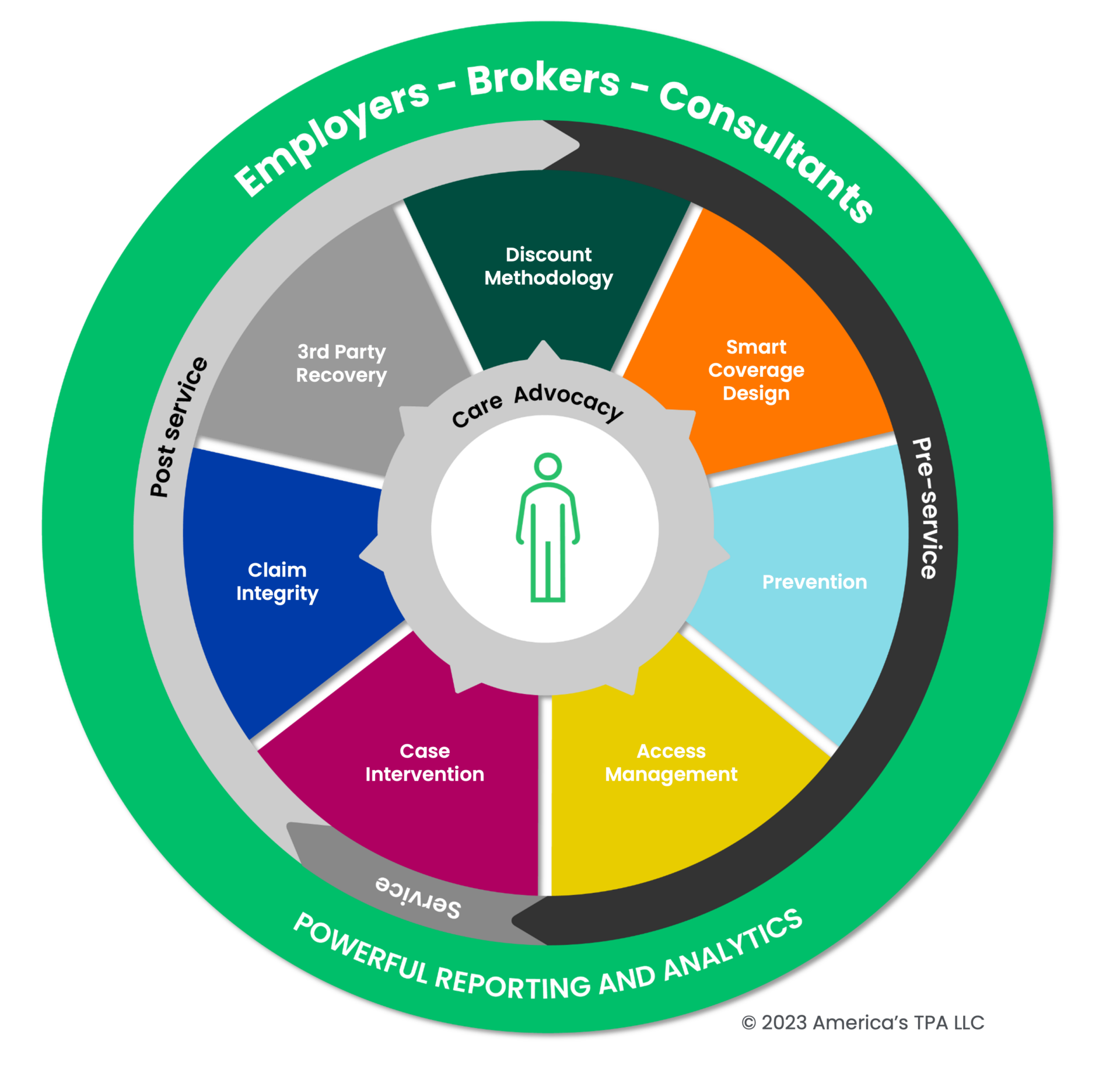
Discount Methodology
• Network Discount
• RBP
• Pharmacy Discounts
• PAP/Manufacturer coupons
• Formulary DiscountsSmart Coverage Design
• 3 Tier Coverage
• Carve Out Programs
• Limitations & Exclusions
• Cost Share StrategyPrevention
• LivEZ – Onsite Biometrics
• Boost Your Baby
• Diabetes Management
• Heart Disease Management
• Weight ManagementAccess Management
• Prior Authorization
• Averted Care
• Advocacy
• Steerage
• Teladoc
• OtherCase Intervention
• Cases Opened
• EngagementClaim Integrity
• High Dollar Claim Review
• Payment Integrity
• Claim Negotiation
• Out-of-Network Discounts
• NSA Savings
• Other3rd Party Recovery
• COB
• Stop Loss
• Subrogation
We’re kind of obsessive
about cost containment
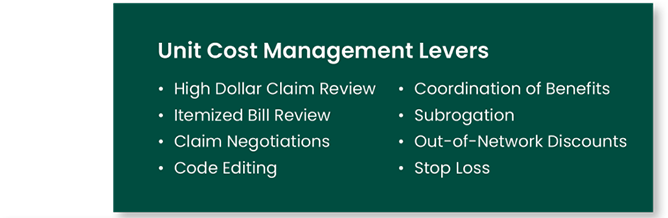
A robust set of tools, levers, and protocols ensure that we can impact cost at every point of service delivery. From plan design to prevention to claims administration to utilization review; if it impacts cost, we have a process in place.

The Power of Care Advocacy:
When you take care of the member,
you take care of the plan.
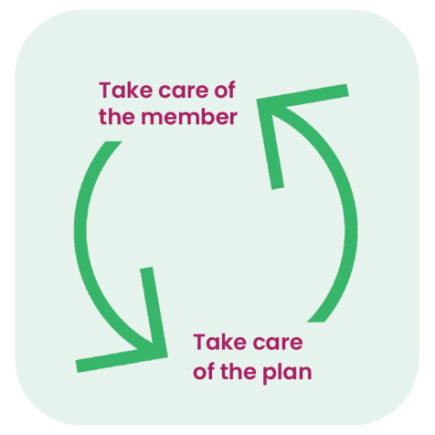
Our member first approach ensures the greatest impact on cost and member experience. Higher member engagement can lead to better outcomes and reduced cost. We provide resources, education, and a review of members’ cases when there is a chronic or complex condition requiring case or disease management. Our team goes the extramile for each member.
• Early identification of potential large claims
• Review for alternative care options
• Early identification of steerage opportunities
To put it simply; caring for the member is good for everyone.

To learn more about our Medical Management team, visit here.

When all else fails, stop-loss
Despite our best efforts, unexpected, big claims can happen. Our in-house risk management team works with A-rated carriers to make sure the plan is covered when the unplanned happens.
We are relentless
We are committed to not only finding cost savings for our clients but also creating a better experience for our members. Generating the savings necessary to make self-funded plans work isn’t easy. That’s why you hire a team like HealthEZ to dig for every possible savings opportunity pre- and post-claim.





